 |
| CM. Flyer. (2018) |
My definition of PTSD would be: PTSD is a disorder in which a person has triggering flashbacks, memories, dreams, or hallucinations about a traumatic event in their past. According to the Veterans Association: "PTSD (posttraumatic stress disorder) is a mental health problem that some people develop after experiencing or witnessing a life-threatening event, like combat, a natural disaster, a car accident, or sexual assault."
PTSD can be very difficult to live with. I wanted to find out what it was like to take care of someone with PTSD. I found an interview with a woman named Rebecca McCoy. Her husband Craig was diagnosed with PTSD. She states, “I basically guide him through each day, do things that he cannot do for himself or help him complete the tasks he cannot finish on his own. I am his primary emotional support, the person who he can talk to openly. I also help him realize and remember that he is worth the fight PTSD brings." This quote shows how hard it is for people who take care of someone with PTSD is. Rebecca and Craig's relationship is much different now that he has been diagnosed with PTSD.
According to the DSM-5 here are 3 criteria for diagnosing PTSD:
Criterion A: stressor
The person was exposed to: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence, as follows: (one required)
- Direct exposure.
- Witnessing the trauma, in person.
- Indirectly, by learning that a close relative or close friend was exposed to trauma.
Criterion B: intrusion symptoms
The traumatic event is persistently re-experienced in the following way(s): (one required)
- Intrusive thoughts: Recurrent, involuntary, and intrusive memories. Note: Children older than six may express this symptom in repetitive play.
- Nightmares. Note: Children may have frightening dreams without content related to the trauma(s).
- Dissociative reactions (e.g., flashbacks) which may occur on a continuum from brief episodes to complete loss of consciousness. Note: Children may reenact the event in play
- Intense or prolonged distress after exposure to traumatic reminders.
- Marked physiologic reactivity after exposure to trauma-related stimuli.
Criterion C: avoidance
Avoidance of trauma-related stimuli after the trauma, in the following way(s): (one required)
- Trauma-related thoughts or feelings.
- Trauma-related external reminders (e.g., people, places, conversations, activities, objects, or situations).
Below is my lesson plan for my simulation. You can follow this so you can also host your own simulation.
For my simulation, I decided to turn PTSD into something good. I didn't want to actually scare anyone or do something that might be traumatic. I decided to ask them about the happiest day of their lives. I asked them to think about all the sensory details they could think of from that day like, what was the weather like, what were the smells, what food did you eat, etc. I had people relax and think about this for a couple minutes. I then told them this is what PTSD could feel like. I then told them about PTSD and why this simulation relates to the disorder. I told them: "What if this day that you were thinking about was the worst day of your life?" I told them that PTSD is like repeating the worst day of your life over and over again. I then had them reflect on the experience and what it would be like to actually have PTSD.
Here is the graph of the expected brain waves of my peers throughout the activity.
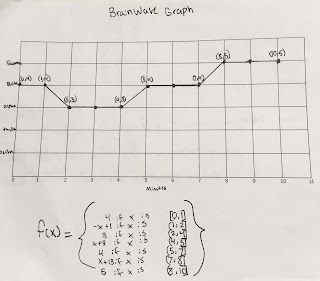 |
| CM 'Piecewise Function" (2018) |
I think that if I had PTSD, daily life could be very hard. I think how difficult would depend on what kind of trauma I had gone through and what kind of triggers I would see in my day-to-day life. I could have a very severe case of PTSD or a rather mild one. I think my life would be different because I would be more anxious than I usually am. I would probably be looking for triggers and seeing how I could get out of situations that might trigger me. I would probably think about the trauma, definitely more than I would like to. I would have to make sure I had time to work my schedule so I could go to therapy to help deal with my symptoms. I might also have to pick up medication like anti-depressants to also help manage my symptoms. I might have night terrors or nightmares about the event that would make me emotional. I would have flashbacks and remember the incident. I would even sometimes be depressed and lose interest in activities and struggle with day-to-day life. I even might be struggling with survivors guilt depending on what kind of trauma I went through in the past. I think my life would be very different if I were having to deal with PTSD. I hope that I will never have to go through it, and if I do, I know the support I need to help get me through this difficult time.
In conclusion, I really liked this project. It was different than the usual projects we do and that was fun. There were a lot of different pieces to the project which did make it hard to keep track of. The part I struggled the most on with this project was coming up with how I was going to simulate PTSD. I talked with my teacher and he helped me with the idea. In the end, I enjoyed this project and have really enjoyed this class. I look forward to the next action project.
Works Cited:
"An Interview About Post-traumatic Stress Disorder: Rebecca McCoy." (2014) Women's Health.gov. U.S. Department of Human Services. Web. 14, March 2018. https://www.womenshealth.gov/blog/spotlight-rebecca-mccoy
Bremner J. Douglas M.D. "Traumatic stress: effects on the brain." National Center for Biotechnology Information. Dialogues in Clinical Neuroscience. Web. 14, March 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181836/
Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, DSM-5, American Psychiatric Association. Washington D.C. (2013) 14, March 2018.
"DSM-5 Criteria for PTSD" (2018) Brainline.org. Bob Woodruff Foundation. Web. 14, March 2018 https://www.brainline.org/article/dsm-5-criteria-ptsd
"PTSD Statistics." (2013) PTSD United.org. Web. 14, March 2018. http://www.ptsdunited.org/ptsd-statistics-2/
"Treating Posttraumatic Stress Disorder."(2018) PTSD Alliance.org. PTSD Alliance. Web. 14, March 2018. http://www.ptsdalliance.org/treatment/
"What is PTSD?"(2018)PTSD Alliance.org. PTSD Alliance. Web. 14, March 2018 http://www.ptsdalliance.org/about-ptsd/





